Healthcare Insights: The Aetonix® Blog
Explore our expert insights on healthcare technology, patient care, and industry trends.
FEATURED BLOG
The Impact of Increasing Health Literacy on Patient Outcomes
Many patients struggle to understand and effectively navigate the healthcare system, which is known as a lack of health literacy. Low health literacy levels are common, with a staggering 60% of Canadians being classified as health illiterate.
Stay Up-To-Date With Aetonix
Interested in receiving updates on healthtech industry insights, case studies, and news about Aetonix and aTouchAway®? Fill out the form below to subscribe to our newsletter.
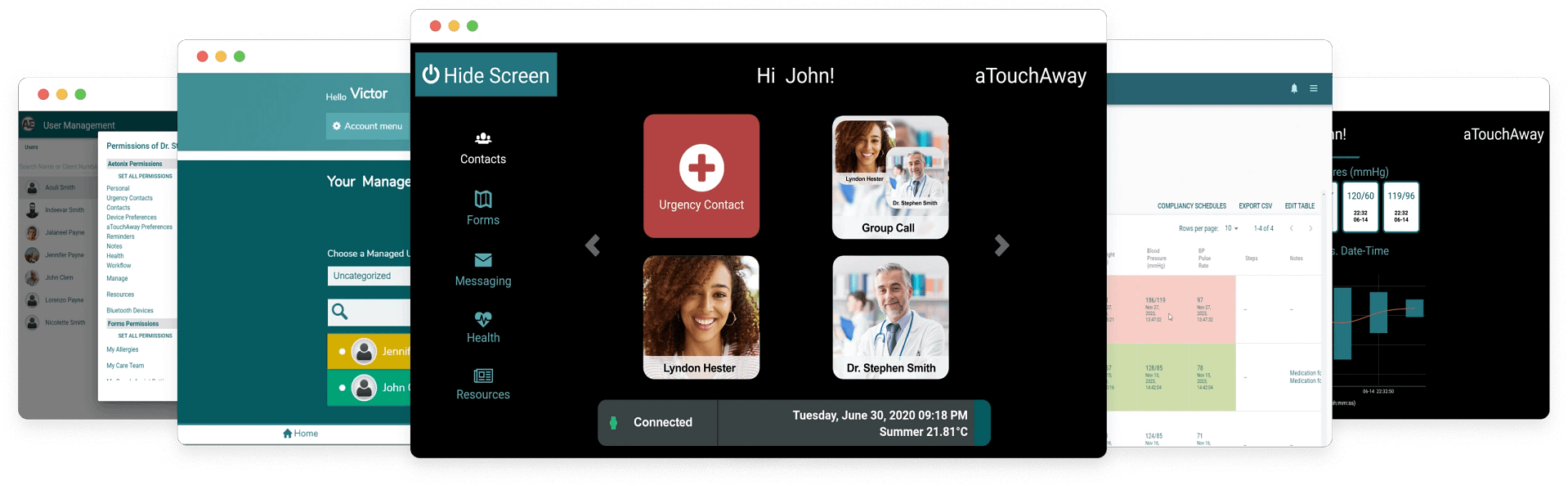
Ready to Explore aTouchAway®?
Book a demo with one of our service specialists and see how aTouchAway can fit into your practice.