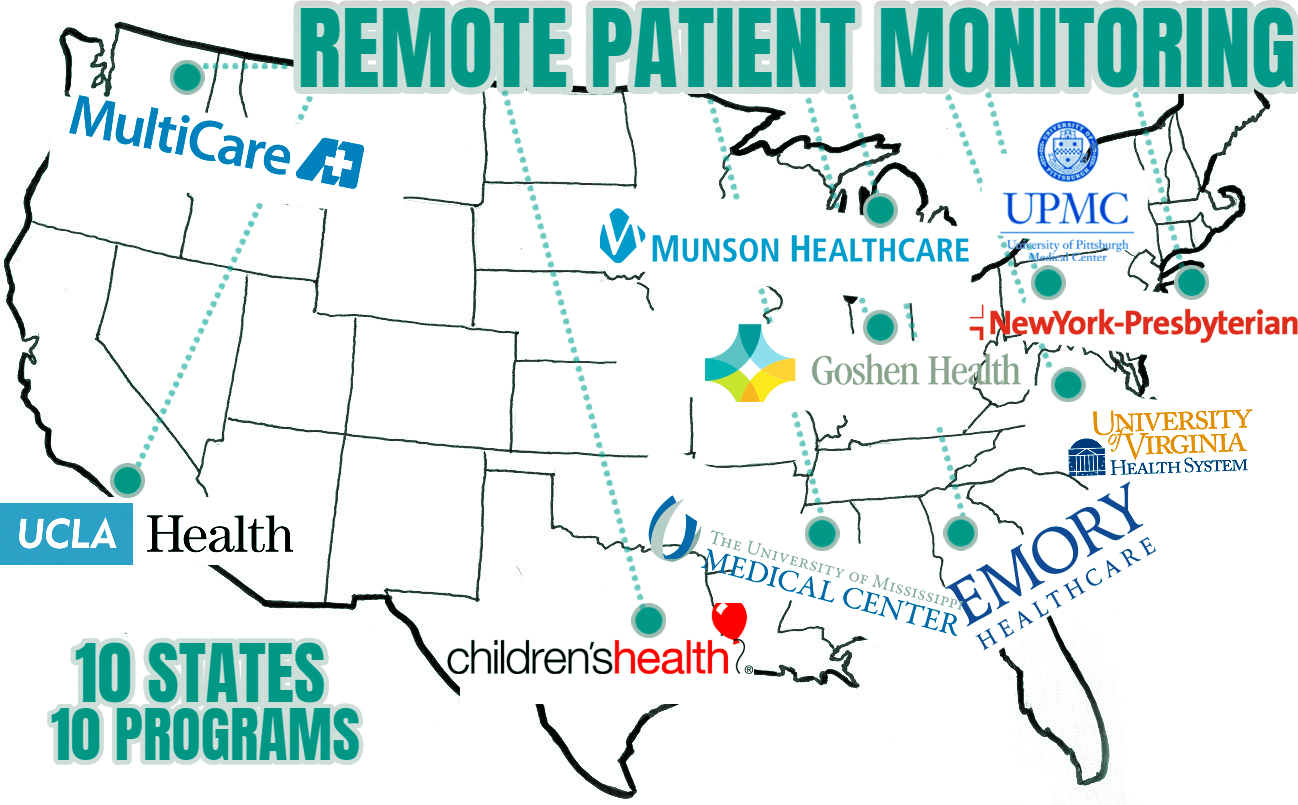
As RPM is such a new space, going through so many legal and technological changes, its value case has overshadowed its use case. Everyone now knows that RPM can add value, but they simply do not know where to begin. Nor do they know what RPM in action looks like. This post is purposefully written for them. I write the Remote Care Intel (RCI), a bi-weekly intelligence report on all things Remote Care. In my research process, I sometimes come across projects undertaken by hospitals and health systems. Thus, I thought it would be a good idea to not just focus on the present, but go back a few years as well, to pull out all the famous RPM case studies that I could find. I have compiled them here. It is very interesting, that the 10 cases were from 10 different states. It just goes on to show how USA as a country, have embraced RPM.
Healthcare is an extremely contextual business. Different organizations have different payor mix, different usage of payment models, and different specialties. So, while it’s good to hear about the benefits of RPM, unless you see how others have done it, you still treat it as an academic concept. These 10 examples will show you that it is very much a real-world concept, applied by hospitals and health systems. Perhaps, one of them will fit your vision of what you thought was possible with RPM.
This article will not cover cases where telemedicine is the only modality. There needs to be some level of monitoring health signals beyond the hospital, for us to consider it as a case of health system deploying RPM. In no particular order, here are the cases.
10. University of California Los Angeles Health System (UCLA Health)
UCLA’s Cardiac Telehealth program monitors patients who undergo heart surgery. Post-discharge, they receive a cardiac telehealth kit. Patients can send the nursing staff daily updates about their recuperation via a questionnaire. They are able to send videos and images of the incision site. Furthermore, daily health indicators are transmitted remotely through devices in the kit. For example, your weight, heart rate, blood pressure and blood oxygen levels can be measured via scale, heart rate monitor, blood pressure monitor and pulse oximeter respectively.
Healthcare providers can immediately detect problems such as shortness of breath, abnormal heart rhythm, adverse reactions to medication, fluid retention etc. With the ability to access such information and conduct video visits as necessary, the success of the recovery process is enhanced. Readmission due to post-surgical complications is reduced.
State: California
Use Case: Wherever there is risk of readmissions, RPM is a very attractive plug in to stop regression and readmission. Post-acute care is one of two major applications of RPM. Chronic care is the other one.
9. University of Virginia Health System (UVA Health)
UVA health has launched multiple RPM programs, geared at chronic care patients. Through its Advanced Diabetes Management Clinic, it tracks patient’s glucose levels, and alerts providers in case of dangerous sways in readings. Also for diabetic patients, retinopathy screenings are conducted remotely via cost-effective screenings. Retinopathy is a leading cause of blindness.
Heart failure patients are given tablets through which they can upload and transmit their vital signs. Through the same tablets, they are also required to participate in a twice-weekly online education and physical activity sessions.
State: Virginia
Use Case: Just two cases in, Chronic Care makes its first, and not last, appearance in the list. And why not? Chronic care is the single biggest market for RPM. It is commendable how UVA is using RPM to not just address chronic care, but screen for specific conditions that can arise from it, such as Retinopathy.
8. University of Mississippi Medical Center (UMMC)
UMMC has a very comprehensive RPM program. It enrolls patients suffering from diabetes, hypertension, heart failure and other chronic conditions into four to six months programs. These programs are customized to the patient’s specific needs, and they are given a tablet which acts as the conduit of the programs. It contains educational material through which they can learn about their conditions, and the best practices to manage them. A UMMC registered nurse regularly checks on the progress of the patients through messaging and video chats, also available on the tablet. The patient is kept up to date on all results. With a provider referral, RPM care is usually covered by the patient’s insurance or Medicaid plan.
State: Mississippi
Use Case: UMMC also treats chronic care, and it emphasizes the care coordination aspect of such care. Nurses carry a lot of responsibility to administer such a program. Indeed, in most chronic care programs, they have the all-important role of being the manager of care plans.
7. Emory Healthcare
Out of Atlanta, Emory Healthcare is doing something slightly more advanced than the typical monitoring of the vital signs. In their RPM program, they are monitoring ECG data through a wearable patch. It has the ability to continuously monitor patients for 72-hour stretches, in both inpatient and outpatient settings. Since the patch stays on the body, and does not need to take a reading manually per se, such continuous monitoring at a stretch is made possible. Coronary heart disease is the subject of this treatment. The autonomic function of patients undergoing angiography is monitored, as prior research has established connection between lower heart rate variability and subclinical myocardial ischemia.
State: Georgia
Use Case: If RPM is a science, cardiology is its greatest source of potential discovery. There are no patient signs which mirror the complicacy of ECG data. Accordingly, some institutions have developed RPM programs just for matters related to the heart, that includes special focus on data analytics.
6. University of Pittsburg Medical Center (UPMC)
UPMC has a heart RPM program very similar to UCLA’s, called Telemedicine Heart Failure. But instead of post-acute care, it is meant for chronic care. More specifically congestive heart failure (CHF) patients. Patients are given a tablet and peripheral devices as a part of a kit. The idea is to have patients manage their illness from the comfort and convenience of their homes, while still having nurses monitoring so they can intervene as necessary. Monitoring the patients in such fashion leads to greater compliance in medication and diet. The kit is given to patients for 90 days. Nurses can ask follow-up questions based on the care plan, or forward patient’s questions or concerns to their physician. Two-way video visits can be started anytime.
State: Pennsylvania
Use Case: CHF is a bit different from other coronary heart diseases because it can be congenital in nature. Thus, often, the patient’s condition cannot be improved, but managed at a reasonable level, which is still better off than exacerbation to worse states. So the focus shifts from just analytics, to more longer term management via various diet, exercise, medication management features. UMPC demonstrates how.
5. Munson Healthcare
Munson Healthcare takes pride in being the only organization in northern Michigan to offer remote patient monitoring services. It advertises it as a great alternative to doctor’s office and home visits. Patients are asked multiple questions every morning on a tablet that they receive. Questions are both qualitative (how they are feeling) and quantitative (heart rate, blood pressure, weight, etc.) Responses are transmitted through a cellular network to the home care registered nurse, who receives it in a designated online portal. It’s the nurses that quarterback such home care, and they can suggest next steps in the form of in-person visits if necessary. Patients themselves can engage in video visits. The tablet is also loaded with education videos surrounding their conditions.
State: Michigan
Use Case: Munson focus on not just treating the disease in question, but changing healthcare practices as we know it. By eliminating both doctor’s office visits, and home care visits, it truly ushers the management of diseases into the digital era.
4. MultiCare Health System
MultiCare has a Telehealth Chronic Disease Management program that connects providers with patients dealing with a variety of chronic diseases, chiefly: heart disease, Chronic Pulmonary Obstructive Pulmonary Diseases (COPD) and pneumonia. The program has approximately 100 nurses overseeing remote care for 80-90 patients per person. The solution is yet again tablet based. It enables caregivers to collect vital signs of the patient, manage their medications, monitor their compliance and also schedule appointments. It is a big jump from how such remote care was conducted before, which was just a phone call.
State: Washington
Use Case: COPD makes an entrance for the first time. Often overshadowed by Congestive Heart Failure (CHF) or diabetes, COPD is just as a big a threat to long term health and well-being as any. Many hospitals and health systems such as MultiCare have it in their strategic long-term vision to tend to COPD, and are already doing so. Often, such programs will sync with existing pulmonary rehabilitation programs, as living with COPD is a big deal to those who have the condition and their family members.
3. Goshen Health
Goshen Health has a telehealth program for chronic diseases such as heart failure, COPD, hypertension and diabetes. They describe the process as first getting a prescription for telehealth services from your physician. Subsequently the necessary devices and technology are installed and explained to you at your home by Goshen Home Care specialists. From there on, your main task is to work the daily measurements into your routine and monitor your vital signs. The home care nurse assigned to you is also there to remotely delegate care.
Goshen’s Heart & Vascular Center also uses remote patient monitoring for post-acute care. After a procedure such as stent placement, pacemaker insertion or cardiac ablation, people need to protect their hearts post-discharge by proper diet, exercise, medication adherence and stress management. They also need to monitor readings from any implanted devices. Through monitoring such implanted devices remotely, it saves the patients time and money. More importantly perhaps, it is more efficient as someone from the care team is continuously monitoring data from pacemakers and defibrillators. Medicare/Medicaid and most insurance companies cover costs for telehealth services.
State: Indiana
Use Case: The technology used for maintaining optimum heart functionality is evolving every day. Similarly, chronic care or acute care programs must keep up so they can remotely extract, monitor and infer from this data. Goshen does a good job in standardizing such cases. Also, COPD makes its second appearance. In reality, most chronic care programs implicitly include the treatment of COPD, even it if is not mentioned.
2. NewYork-Presbyterian Hospital
NewYork-Presbyterian is no stranger when it comes to remote innovation in healthcare. It previously made headlines for its teleparamedics and telestrokes unit. Everything is on board in the ambulance including the virtual presence of specialists, lifesaving medication and all equipment that is necessary to conduct any relevant tests. It is remote acute care at its best.
More recently, New York Presbyterian has expanded its virtual care capabilities with remote patient monitoring. Physicians can now monitor patients’ vital signs and send them short questionnaires on their health status. Patients from their end can remotely transfer their vital signs using devices that is connected to a tablet. Thus, they too, have joined the act on chronic care.
State: New York
Use Case: Remote care is great for solving the most urgent problems due to the frequency of access and speed it provides to those in need. When ambulatory care is not fast enough, remote care helps by possibly preventing life threatening situations. With the shift to population health management, more is being done to prevent emergency situations in the first place. So yes, if it was anyone providing chronic care, NewYork-Presbyterian would be one of the first institutions to come to mind.
1. Children’s Health
Children’s Health, out of Dallas, has a comprehensive pediatric RPM program. The pilot RPM program consisted of 50 pediatric patients of various ages, who were dealing with organ transplants. The RPM platform helped adolescent patients adhered to complicated medication regimens. Previously they also had rolled out a neonatal RPM program, where infants could be monitored wirelessly, and their cases could be consulted virtually. Zooming out of the home, they also set up digital care points in the form of kiosks at retail pharmacy locations.
State: Texas
Use Case: With this example, the third major form of care to embrace RPM makes an entry, that is neonatal care. In Neonatal ICUs, health indicators are absolutely essential, and it just makes it easier if it can be done remotely via sensors. For those children who are older and suffering from various complications, it helps that they are more tech savvy, thus RPM is a great way to provide care to such a population.
I hope you enjoyed reading the article. If you have any questions/suggestions, please reach out to me at rahat.haque@aetonixsystems.com. Also make sure to follow our Social Media pages above. We would love to hear from you.
We are Aetonix. We Simplify Complex Care.
References
https://www.umc.edu/Healthcare/Telehealth/remote-patient-monitoring-for-providers.html
https://www.upmc.com/healthcare-professionals/physicians/telemedicine/services/remote-monitoring
https://www.munsonhealthcare.org/about-the-system/news-media-relations/news/news-details?news=693
https://goshenhealth.com/health-library/telehealth-services
https://medcitynews.com/2019/01/newyork-presbyterian-hospital-philips/?rf=1
https://www.childrens.com/specialties-services/remote-patient-monitoring