Remote Patient Monitoring (RPM) is rapidly becoming a cornerstone of healthcare, propelled by the digital transformation that’s reshaping patient care delivery. RPM, a pivotal component of telehealth, leverages digital technologies to monitor and capture medical and other health data from patients remotely. This data is then electronically transmitted to healthcare providers for assessment and, when necessary, instructions are sent back to the patient. As healthcare systems strive to improve patient outcomes, reduce healthcare costs, and enhance patient convenience, RPM stands out for its potential to meet these goals efficiently.
Comprehensive Breakdown of RPM Costs
Initial Considerations
Embarking on an RPM initiative requires a clear understanding of the specific needs it aims to address. Whether it’s managing chronic conditions, improving patient engagement, or reducing hospital readmissions, identifying these goals upfront can significantly impact the choice of RPM technologies and, consequently, the costs involved.
Direct Costs of RPM
Hardware: The cost of RPM devices, such as wearables, blood pressure monitors, and glucose meters, can vary widely based on the sophistication and intended use. Factors influencing costs include device accuracy, battery life, and brand reputation.
Software: Investment in RPM platforms includes costs for patient portals, data analytics, and integration capabilities with Electronic Medical Records (EMR). The choice of software can significantly affect both upfront and ongoing costs.
Services: Initial setup, integration with existing healthcare IT systems, and training for both healthcare providers and patients are essential services that incur costs. Additionally, ongoing support and maintenance are crucial for the long-term success of any RPM program.
Operational Costs
Maintenance and Updates: Continuous operation of RPM systems requires regular software updates and device maintenance, contributing to the operational costs.
Subscription Models vs. One-time Fees: Some vendors offer RPM software and services on a subscription basis, while others may charge a one-time fee. The choice between these models can affect the program’s long-term financial sustainability.
Connectivity Costs: Ensuring reliable data transmission between patient devices and provider platforms can involve expenses related to cellular services or internet connectivity, especially in remote areas.
Hidden and Indirect Costs
Customization and Scalability: Customizing RPM solutions to fit specific clinical needs or scaling the program to accommodate more patients can incur additional costs.
Interoperability Issues: Ensuring that RPM systems can seamlessly exchange data with other healthcare IT systems may require additional investment.
Patient Engagement Strategies: Effectively engaging patients in using RPM technologies involves costs related to education, training, and ongoing support.
Strategies for Cost Management and Optimization
Buy vs. Lease Analysis
Deciding whether to buy or lease RPM equipment is crucial. Leasing can reduce upfront costs and provide flexibility to upgrade technologies as they evolve. However, purchasing equipment might be more cost-effective in the long term, particularly for large-scale deployments.
Exploring Open Architecture
Opting for RPM solutions with open architecture can reduce costs by ensuring system interoperability and avoiding vendor lock-in. This flexibility allows healthcare providers to mix and match devices and software, potentially lowering costs and facilitating future upgrades.
Understanding Pricing Models
Navigating the various RPM pricing models is essential for cost management. Transparent pricing models that clearly outline what is included in the subscription fee, such as device costs, software access, and support services, can help in making informed decisions.
Measuring Return on Investment (ROI)
Assessing the ROI of RPM programs involves looking beyond direct costs to consider the broader benefits, such as reduced hospital admissions, improved patient outcomes, and higher patient satisfaction. Real-world case studies demonstrate that RPM can offer significant returns by improving health outcomes and reducing overall healthcare costs.
Cost Summary Table
Since direct source references for these estimations aren’t provided in real-time or based on a specific database, the references column will indicate the type of sources typically consulted for such information. It’s important for anyone interested in RPM costs to consult with vendors, industry reports, and healthcare IT consultants for the most current and applicable data.
|
RPM Component |
Cost Range (CAD) |
Notes |
References |
|
Hardware (Devices) |
$200 – $5,000 per device |
Includes wearables, blood pressure monitors, glucose meters, etc. Price varies by device type and features. |
Vendor quotes, product catalogs. |
|
Software (Platform) |
$5,000 – $20,000 initial setup + $300 – $1,500 monthly subscription |
Costs depend on the complexity, scalability, and specific features required (e.g., data analytics, integration capabilities). |
Vendor proposals, software product listings. |
|
Services |
$2,000 – $10,000 initial setup + variable ongoing fees |
Setup, training, integration, and support services. Ongoing costs depend on the level of service required. |
Service agreements, vendor service packages. |
|
Maintenance & Updates |
$500 – $3,000 annually |
Regular software updates and hardware maintenance fees. |
Maintenance contracts, vendor service agreements. |
|
Connectivity |
$20 – $100 per patient/month |
Costs for cellular or internet service required for data transmission. |
Telecom service providers, data plan pricing. |
|
Customization & Scalability |
$1,000 – $15,000 |
Additional costs for tailoring the RPM solution to specific needs or scaling the deployment. |
Custom development quotes, scalability planning estimates. |
|
Interoperability |
$500 – $5,000 |
Costs to ensure RPM systems work seamlessly with existing healthcare IT systems. |
Integration service quotes, software interface development costs. |
|
Patient Engagement |
$1,000 – $5,000 |
Education, training, and support for patients to effectively use RPM technologies. |
Patient education program costs, training materials and sessions. |
|
Subscription Models |
$300 – $1,500 monthly per 100 patients |
Often includes access to both patient and provider platforms, with prices varying by features and scale. |
Subscription service agreements, vendor pricing models. |
|
Lease vs. Purchase |
Variable |
Leasing can reduce upfront costs but may result in higher long-term expenses. Purchasing requires a higher initial investment but can be more economical over time. |
Financial analysis, vendor leasing agreements, purchase contracts. |
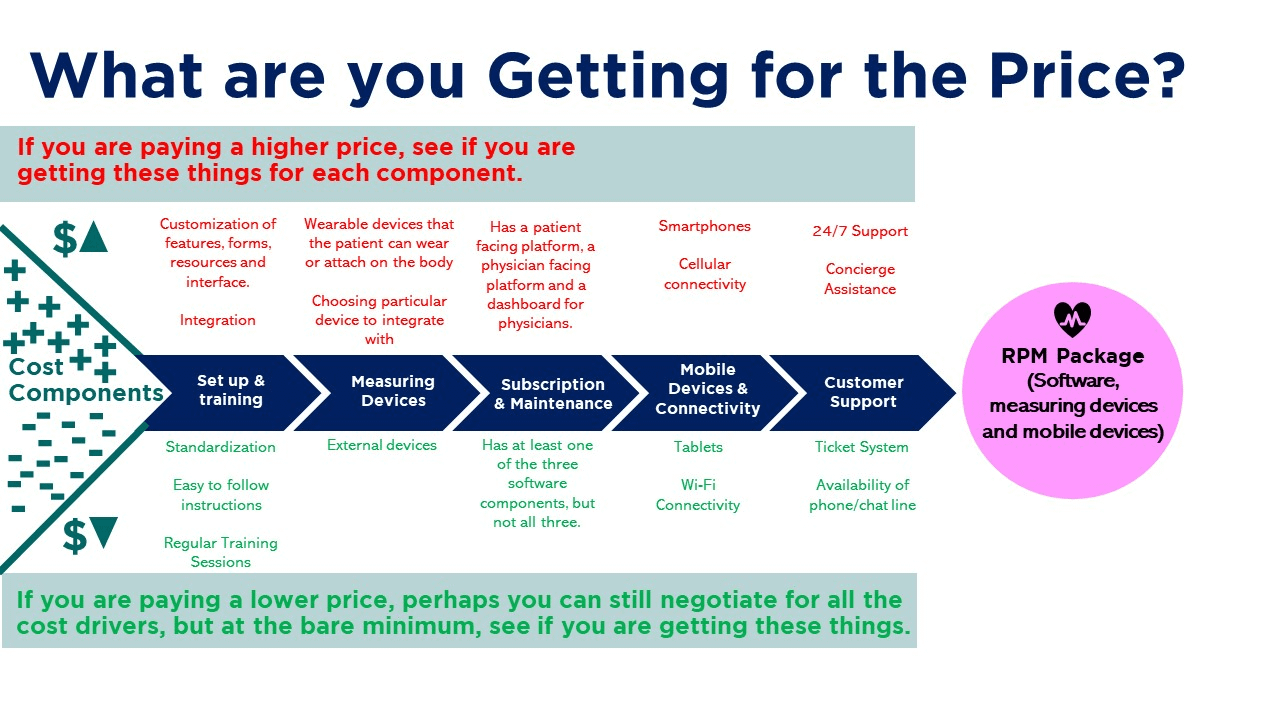
Cost Components and RPM Package
 Future Trends and Cost Implications
Future Trends and Cost Implications
Emerging technologies, such as AI-driven analytics and next-generation wearables, promise to enhance RPM’s capabilities and effectiveness. However, these advancements might also introduce new cost considerations. Additionally, evolving healthcare policies could impact reimbursement for RPM services, affecting program sustainability and financial models.
Conclusion: Making Informed Decisions
Investing in RPM is not merely an operational expense but a strategic move towards improved healthcare delivery. Understanding the comprehensive costs involved—from direct hardware and software expenses to indirect costs related to patient engagement and system interoperability—is essential for making informed decisions. As RPM continues to evolve, staying informed about the latest trends and cost management strategies will be key to maximizing the benefits of this transformative healthcare approach.
Thank you for exploring the complexities of RPM costs with us. For more insights into digital health and RPM technologies, consider subscribing to our blog for updates and in-depth analyses.

 Future Trends and Cost Implications
Future Trends and Cost Implications