At this crucial time for world health due to the COVID-19 pandemic, Aetonix is proud to collaborate with our partners across the Atlantic in UK, to enable the Life Lines ICU Project.
What is Life Lines?
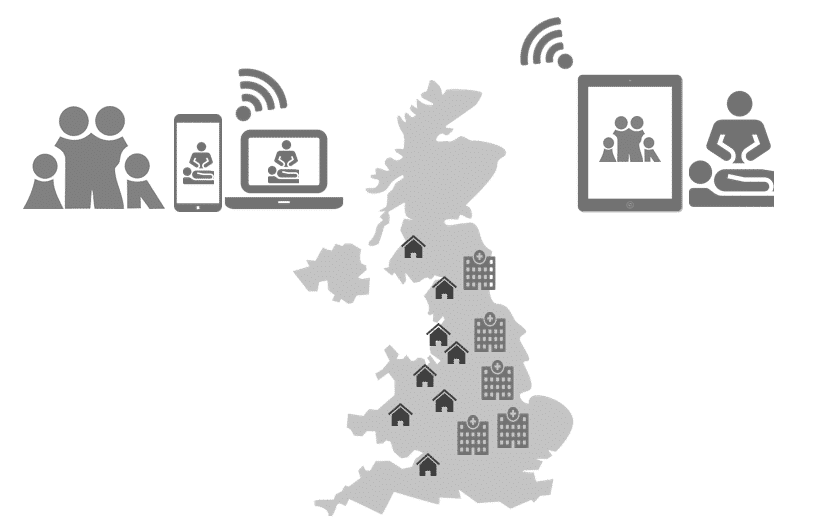
The Life Lines ICU project enables healthcare staff to connect families with critically ill patients through a virtual visiting solution from aTouchAway®. It is deployed on thousands of 4G-enabled BT tablets distributed into ICUs across the UK for COVID-19. Please visit the Life Lines website for more information on the genesis of such a project, the different partners that are involved and how you may help.
The Build up
Currently, due to the threat of influx of symptomatic patients, healthcare is being prioritized according to each person’s level of need. As a basic first step, healthcare organizations are encouraging patients to remotely self screen themselves via questionnaires, so they can be triaged virtually without needing to come to a physical location. We have created such a feature ourselves to enable our current clients. For patients who need further care or in location testing, they are being transferred to specialists who may have a better look at their case. Special arrangements such as walk in testing or drive through testing are also being arranged. But for those patients who need urgent in person care, and reach a critical stage, they are of course transferred to ICU units, and isolated from the rest of the world apart from the clinicians that provide care. Hospitals are ensuring that they have enough capacity to treat those who are at this critical stage, or at risk of getting there.
The Purpose
Life Lines was envisioned in order to serve those who have already reached the stage of ICU lockdown, and are separated from their family members due to the contagious nature of COVID-19. Such a disconnect in communication can have great psychological impact for both the family members and the patient. There is also the chance of fatality, in which case the need for communication is even more palpable. In order to bridge this gap in communication, Life Lines stepped up to fill the void where ICU staff could add patient’s family members and communicate with them in order to schedule a video call. The user experience from the family member’s side is very intuitive where they are given a registration link, that takes them through all the steps to download the app, and communicate with the ICU staff.
The prestigious King’s College London, UK, approached us with the Life Lines program, seeking a partner that would help them bridge the communication gap between family members separated at this critical time. Given that we already had a secure and fully compliant video call solution in place, which could also be customized according to the particular use case, we gladly obliged. After our pilot at London’s St. Thomas hospital, this solution is being rolled out at ICU units of the rest of UK as well.
CONTACT LIFE LINES in UK
If you are in UK, and you are interested in the solution or in a collaboration, please send all queries to LifeLines@kcl.ac.uk
If you want to support the further expansion of Life Lines, please consider making a donation here.
Follow Life Lines on Twitter for all the latest updates on the project.
LET US DO THE SAME FOR CANADA
If you are in Canada or USA , and you are interested in the solution or in a collaboration, please send all queries to rahat.haque@aetonixsystems.com
READ BELOW ON HOW WE CAN STAY PREPARED IN NORTH AMERICA BY HAVING VIRTUAL COMMUNICATION IN PLACE
Let’s take a look at the latest case numbers from the three countries we currently operate in: *As of April 7th*
| Country | Total | Total | Total | Total | |||
| Cases | Deaths | Recovered | Critical | Fatality Rate | Recovery Rate | Critical Rate | |
| USA | 363,353 | 11,038 | 19,247 | 8,830 | 3% | 5% | 2% |
| UK | 55,410 | 5,812 | 135 | 1,559 | 10% | 0% | 3% |
| Canada | 16,194 | 306 | 3,128 | 426 | 2% | 19% | 3% |
In the coming days, you can expect the recovery rate to shoot up as the majority of the total cases are still active cases. But the fatality rate and the critical rate thus far have been alarmingly high. In the coming weeks, the ICUs of USA and Canada could undergo the same fate as they did in UK, with the fatality rate peaking out at 10%. For these times, a virtual connection solution would go a long in way in providing the type of communication support and solace families are looking for. If you anticipate such needs, please do get in touch with us.
Aetonix as a company has always prided itself in providing a continuous stream of care to those patients with complex needs, such as suffering from multiple chronic diseases, or needing pre and post operative coordination, etc. COVID-19 is the latest in line of such use cases, where we do not want to merely focus on prevention and case management, which we do via remote screening and virtual assessment in USA and Canada, but we also want to focus on those who are already at a critical stage. Along with our partners in UK, we are here to serve their needs through Life Lines. We want to replicate such a project in Canada if possible. Let us connect if you plan on making this a reality.