Mitigate Further COVID-19 Spread
Remotely Screen your Patients for Free in Canada Using aTouchAway®
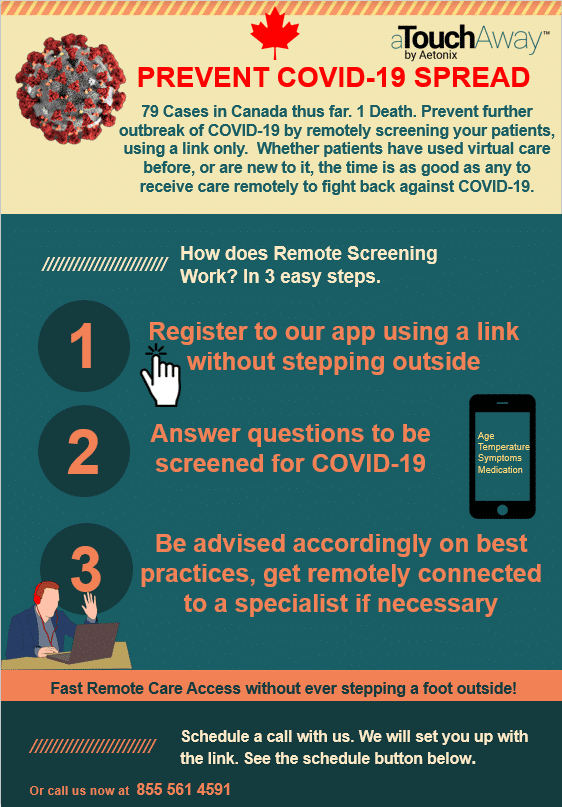
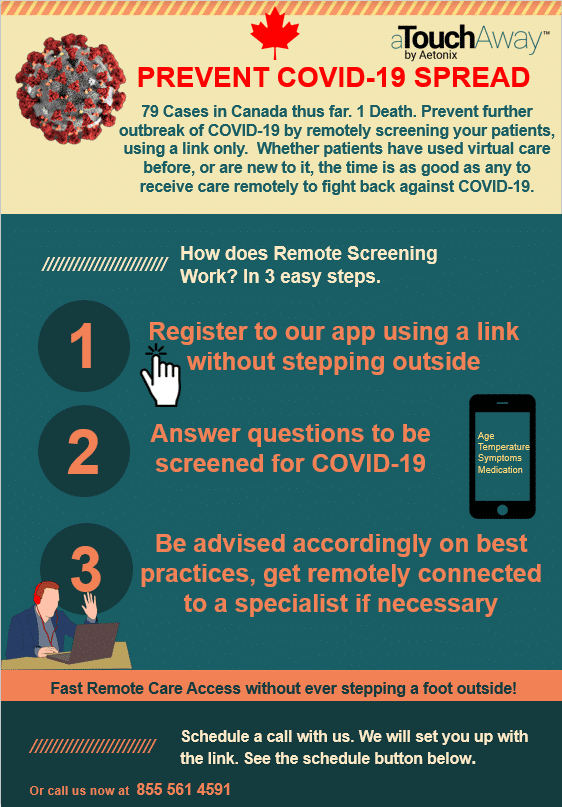
Canada hasn’t had it as bad as some other countries. But things could spiral out of control very quickly, if prevention measures are not enacted. In light of the COVID-19 breakout, Aetonix is making the use of aTouchAway free for a couple of months for remotely screening potential COVID-19 cases.
It can be as easy as sending a link to your patients, whether you are a hospital, Nursing Home or a long term care agency. From there on, they could be remotely screened using a series of questions, connected to physicians if necessary, or even specialists in case of escalations. All this inside the privacy of their own homes, so further contagion is prevented.
Aetonix Systems Inc. started delivering remote care to patients in 2014, and was ahead of its time when all the legislation regarding telehealth and remote care was still being settled. Now in 2020, with its years of helping hospitals in Canada build remote care programs under its belt, it is positioned to help fight back against COVID-19.
* Refer to the brochure below on the simplicity of the remote screening process. Note that the case toll was from March 10th, for a more recent count, please refer to the Track the Outbreak link under helpful resources.
Response
Prime Minister Trudeau pledged a $1.1 billion fund to fight the COVID-19 that includes spending on a variety of activities. Such as immediate public health response, support for provinces and territories, work sharing programs, etc. Clinics have been set up in all affected areas to test for the virus, returning Canadians with COVID-symptoms are being quarantined on Canadian soil, before being reintegrated to society. University of Toronto developed a disease transmission model that predicts that the virus could affect a minimum of 35% of Canadians provided if half of the mild cases were identified and isolated. Individuals are advised to call their public health authority hotlines if they are symptomatic of the condition.
Ontario Reimbursement
Effective on March 14th, the Ministry of Health and Ontario Medical Association have created three temporary codes that enable virtual screening of patients via telephone and video.
Temporary Codes
K080- minor assessment of a patient by telephone or video, or advice or information by telephone or video to a patient’s representative regarding health maintenance,diagnosis, treatment and/or prognosis. $23.75
K081-a. intermediate assessment of a patient by telephone or video, or advice or information by telephone or video to a patient’s representative regarding health maintenance, diagnosis, treatment and/or prognosis, if the service lasts a
minimum of 10 minutes; or
b. psychotherapy, psychiatric or primary mental health care, counselling or interview conducted by telephone or video, if the service lasts a minimum of 10 minutes $36.85
K082- psychotherapy, psychiatric or primary mental health care, counselling or interview conducted by telephone or video per unit (unit means half hour or major part thereof) per unit $67.75
K083- Specialist consultation or visit by telephone or video payable in increments of $5.00
COVID-19 Sessional Unit
H409 per one hour period, or major part thereof $170.00
For further clarification, refer to the following bulletin.
Ontario has implemented enhanced Measures to Protect Ontarians from COVID-19, which includes enhanced access to screening.
British Columbia Reimbursement
The BC government and Doctors of BC have agreed that consultations, office visits, and non-procedural interventions where there is no telehealth fee may be claimed under the face-to-face fee with a claim note record that the service was provided via video technology or telephone are payable by MSP.
In addition, the General Practice daily volume limits are suspended. Services directly related to COVID-19 should include diagnostic code C19.
For a full list of BC’s telehealth/virtual care codes, see here.
Quebec
As of yesterday (March 16th), General practitioners in Quebec will be able to conduct consultations by telephone or virtually. Doctors in Quebec are encouraged to use this practice by The Fédération des médecins omnipraticiens du Québec (FMOQ) and also the government.