Why Care Transition Matters
In a time when the patient journey involves increasingly rapid transitions between care settings, accurate communication—with tools that facilitate clear, accurate information exchange—has never been more important. The average length of a hospital stay has decreased due to downward pressure from operational costs and improvement in outpatient care. In healthcare systems around the world, the length of hospital stay is used as an indicator of healthcare quality, so hospitals are motivated to discharge patients as soon as they’re ready.
But this impetus for a quick discharge carries dangers—not least that the patient will end up returning to the hospital with the same symptoms, or in worse condition than before. That’s why care transition is so important: it ensures continuity of care as the patient moves from one setting to another and accountability is transferred from one care team to another.
If care transition is not done right, the health system risks not only bad patient experiences but increased pressure on the system in the form of readmissions. In the United States, 20% of Medicare patients return to the hospital within 30 days, costing more than US$26 billion annually. In Canada, around 9% of patients are readmitted to the hospital within 30 days of discharge, costing C$2.1 billion a year. For the UK, this figure is 8%, causing the NHS £1.6 billion per year. Clearly, there’s room for improvement.
Focusing on the Hospital-to-Home Transition
The most frequent care transition that occurs is from hospital to home, so the biggest potential for impact lies in improving this one transition.
A study published in JAMA Internal Medicine found that patients discharged into home health care had a higher readmission rate than patients discharged to a skilled nursing facility. The study considered these two post-acute care settings because 90% of Medicare patients are discharged into one of these settings. It’s not hard to guess why home care had a higher readmission rate: patients at home don’t receive the intense round-the-clock care that they would get in a skilled nursing facility.
The home is an unstructured, unsupervised setting. More than in any other setting, the patient has a high degree of accountability. If patients will require help from caregivers or services from community organizations, those needs must be assessed and explained to them before they walk out the hospital doors.
A Simple 4-Step Model for Discharge
Creating and implementing a clear discharge plan is key to transitioning patients from hospital to home without further complications or readmission. Slight differences exist between various care transition models that have been tested. But usually, these models address active issues, required services, warning signs to look out for, and whom to contact 24/7 in the case of an emergency.
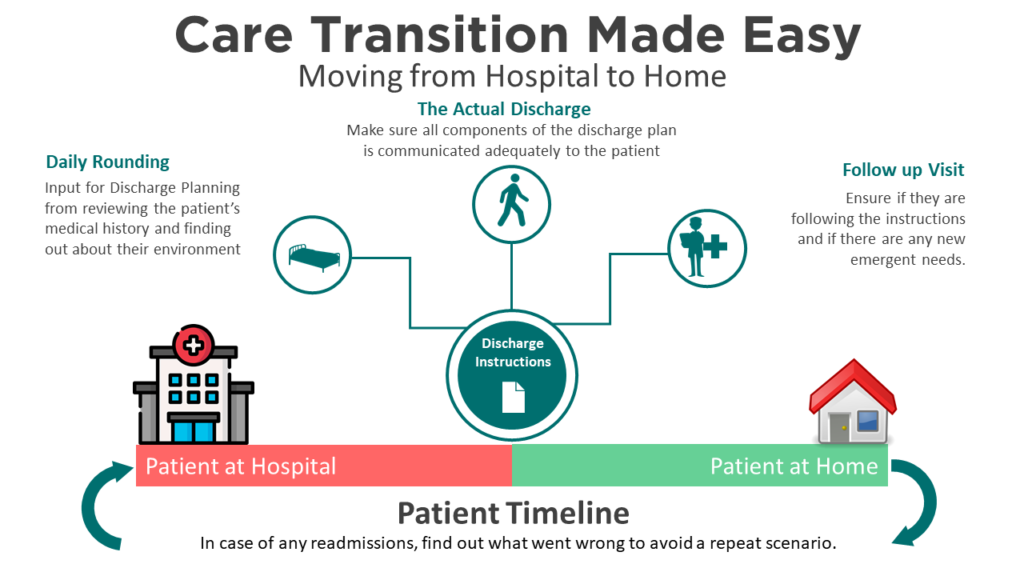
There are four steps to the discharge planning process:
- Gathering information for the discharge plan through daily rounding
- Clearly communicating the plan to the patient at the time of the discharge
- Conducting a follow-up visit to assess compliance and any need for changes to instructions
In the case of readmission, assessing what went wrong and revising the plan
1. Daily Rounding: Gathering Information for the Discharge Plan
Rounding is the process of visiting patients to have meaningful conversations about their status, to explain the care they have been receiving and uncover areas for improvement. It has become a nursing best practice over the years.
Rounding is an opportunity to teach the patient how to handle self-care and self-manage medications. By conducting such a process daily, or at more frequent intervals where necessary, healthcare professionals can also begin to assess risks such as low literacy, presence of other conditions, other recent readmissions, medication history, etc. By looking at the patient’s electronic health record and by interviewing them when they are able to speak, professionals can assess their social and economic situation. This information is then used to assemble a post-acute care transition plan that puts everyone on the same page.
At this stage, it’s crucial to exchange information electronically with all those who need to be involved in the patient’s care. Any primary care physician should be identified by name, as should any nurse, social care worker, or informal caregiver who will be visiting or caring for the patient. It’s best to assign a coordinator or navigator who can be the first point of contact for the patient. Once all such input is gathered and verified, it’s possible to finalize the care transition plan and disseminate the information via a discharge meeting.
2. Communicating the Discharge Plan
When a patient transitions from the hospital to another care setting, the discharge plan is the preferred way to lay out what comes next. It is an agreed-upon outline of the next steps and expectations of all parties. Systematic reviews have shown that enhanced discharge planning is a contributing factor to lower readmissions. During discharge, instructions are reviewed with the patient. The plan educates them on their diagnosis and the extent of the evaluation performed on them. It also outlines a medication management plan, any follow-up visits where they have to see their primary physician, and a scheduled home visit from a nurse and/or social worker.
It’s crucial to make sure that the patient—or someone responsible for the patient—understands the discharge instructions and can follow them. Explain the information to the patient in their preferred language, and use pictures to reinforce the message if necessary. Patients may be unable to remember such sessions if they are not in the right mindset, or because they have undiagnosed dementia. Social factors could also prevent patients from understanding and adhering to the plan. Some may not be able to read or may not have the money to pay for medications.
In short, no assumptions should be made when the patient is ready to leave the hospital. An estimated 80% of serious medical errors happen because of miscommunication during the hand-off between medical providers. It is the responsibility of the incumbent healthcare professional not only to explain to the patient what is about to happen, but also to update their care provider, usually the primary care physician.

3. Following Up
Follow-up visits are common in all care transition models. Nurses from the patient’s primary physician’s office or home care agencies must make sure the patient is taking their medication in the correct dosage. They must assess whether furniture in the house presents fall hazards and whether the patient needs any supportive furniture like bathroom safety bars. They must also determine whether the patient has proper access to transportation, meals, caregivers (if needed), etc.
4. Closing the Loop
If readmission does occur, it is important to find out what caused it, to avoid repeating the pattern. Even with a well-thought-out and clearly communicated discharge plan, some problems may have been overlooked. In such instances, corrections can be incorporated into the next discharge plan.
Finally, it’s important to collect the patient’s feedback on the quality of the transition of care. Healthcare is a two-way street, and to achieve full engagement and cooperation from patients, it’s necessary to hear their side of the story.
Many thanks for reading. If you haven’t already, please consider subscribing to our blog by going to our blog page and scrolling down to the subscribe form. Feel free to share this post on your Social Media channels by using the share buttons at the bottom of this page.

