A Critical Need for Communication
In the urgency of a critical care setting, communication is a key—but often overlooked—factor in both the patient experience and the effectiveness of care. In this setting, virtual care solutions can make a tremendous positive difference.
Critical care refers to the treatment patients receive in intensive care units (ICUs). All large hospitals have ICUs that house patients whose condition is life-threatening or unstable. Critical care is synonymous with intensive care, where patients receive comprehensive round-the-clock care to stabilize and manage perilous conditions.
Admission to the ICU for critical care is reserved for patients who have one or more impaired organs, or who require respiratory support. Directors of critical care and ICU directors in health systems are responsible for managing the patient experience in such settings.
When done right, communication in a critical care setting improves patient outcomes, boosts psychological recovery, and increases the satisfaction of both the family and the patient. These benefits have been clear in connecting ICU patients to their families during the COVID lockdown.
Communication Challenges in the ICU
Communication in critical care settings poses a range of challenges, including language comprehension, cultural differences, and dealing with the stress of the situation.
Indeed, half of all family members of ICU patients report communication with physicians to be inadequate. Almost three-quarters report confusion over what is communicated to them.
One of the unique challenges of communication in a critical care setting is that the patients themselves are often unable to communicate because they are sedated or intubated. Nearly 95% cannot give consent to invasive therapies, such as being put on life support or having an operation performed. Thus, it is up to the healthcare team to communicate among themselves, and with the relatives of patients.

Where to Start?
If you’re interested in putting together a communication strategy for your ICU, it’s easy to get lost in the weeds. There is a lot of medical advice out there about talking to ventilated patients. We won’t get into that, but here’s a great algorithm for what to do in such a situation.
Rather, we’ll focus on the other two communication scenarios that are more frequent in such a setting. These are communication among healthcare professionals and with the caregivers and families of patients.
A successful communications model for critical care includes policies to improve communication on both these fronts. And in both cases, virtual care can facilitate stronger communication, whether through sharing notes, scheduling appointments, or providing greater accessibility.
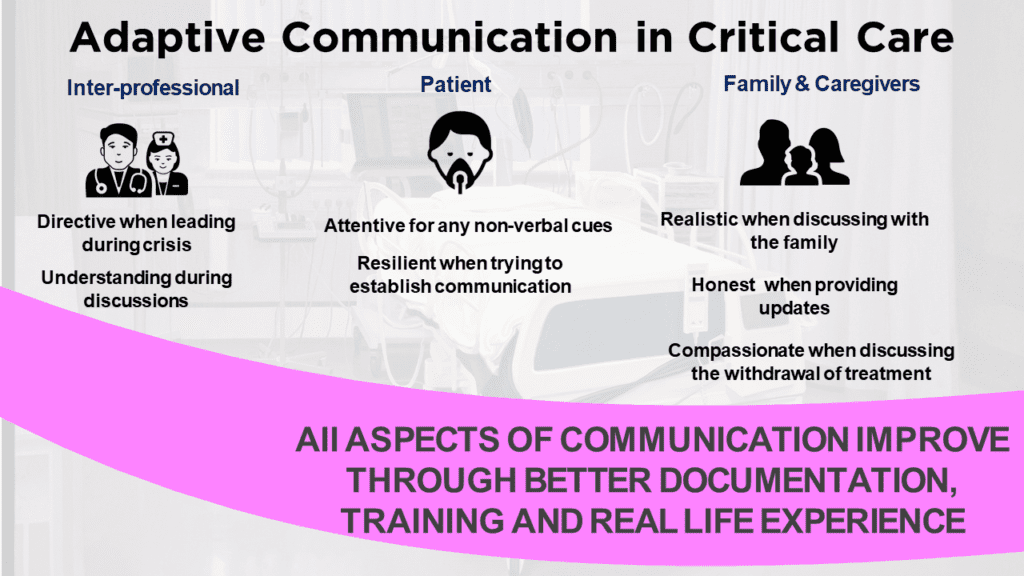
Adaptive Communication
Adaptive communication means shifting “modes” to communicate effectively with different people in different situations.
As the objective is to get the patient out of the ICU as soon as possible, it is easy to rush communications. But clear and effective communication is in fact key to reducing the length of an ICU stay while promoting the best outcomes.
During a patient’s stay in the ICU, team leaders need to apply a number of different communication modes. They must:
- Direct during a crisis
- Listen to arguments and handle disagreements during inter-professional discussions
- Exercise patience when talking to an intubated patient
- Convey information clearly when discussing with the family
- Be realistic when explaining the prognosis
- Be honest when providing updates
- Be compassionate if negotiating the withdrawal of treatment plans
That’s a lot of different communication skills, all for the same case!
Thus, an adaptive mindset is crucial. Leaders can best act according to the situation if they have built the temperament for it through training. But as a starter, they can simply recognize that they may have to adapt their tone and behavior throughout the care process.
Inter-professional Communication
In ICUs, 37% of errors are due to poor communication between physicians and nurses.
Interventions available to reduce such errors include the daily goal sheet and bedside dashboards. The daily goal sheet includes tasks to be completed, the care plan, and the communication agenda for the day. Bedside dashboards include progress notes and document the status of daily goals. Door communication cards, posted on the door of the patient’s room, are used for the same purpose but are not as effective as the other two measures.
If you’re designing a communication strategy, make sure you include at least one of these measures—and the more, the better. Many templates are available to document communication and close the communication loop between physicians and nurses. If you have a virtual care platform in place, you can create such protocols and include it as a part of your intensive care pathway.
In addition to following strong documentation practices, all staff must be trained at a group level if the organization is serious about improving the quality of interactions and aligning goals between physicians and nurses. Team training is better than individual training, as it better replicates real-world scenarios, where healthcare professionals have to interact with each other.
Multidisciplinary team training increases trust and respect for each other’s role in healthcare. Multidisciplinary shift evaluations—where at the end of the shift, all staff gather to discuss what they did right and what needed to improve—increase team accountability. It is possible to conduct such meetings virtually, using a virtual care platform that allows members of the care team to collaborate on a patient’s case.
Family & Caregiver Communication
During the distressing time of a family member’s illness, family meetings are an essential aspect of healthcare professionals’ responsibilities. Many experts think that conducting family meetings should be treated as a procedure, with some even saying that it requires no less skill than an operation.
While other medical aspects in critical care are following procedures, such as sedating a patient or inserting catheters, the same level of training is not provided for communicating with the family. Learning about communication both via formal training and also by observing others leading the family meetings can improve the quality of family communication. To formalize the family visit, it can be included as an event in a patient’s intensive care pathway.
Non-verbal communication is very important in critical care. Nurses must not hesitate to provide physical comfort, such as consoling the caregivers and families when a prognosis is not looking good. They can also find themselves on the receiving end of the backlash caused by the fear and anxiety of the patient’s family or caregivers. Through training and direct experience, the staff is expected to find a balance between maintaining boundaries and recognizing the family’s needs.
Finally, proper scheduling is important. Enough time must be allowed for each family meeting so that the process is not rushed. With digital scheduling, visits can more easily be planned and spaced out in advance.
Many thanks for reading. If you haven’t already, please consider subscribing to our blog by going to our blog page and scrolling down to the subscribe form. Feel free to share this post on your Social Media channels by using the share buttons at the bottom of this page.

