Understanding Obstacles to Healthcare Access
Patient access is one of the universal markers of a great healthcare system, along with value and care experience. It’s also one of the toughest to achieve—and an important application of telemedicine.
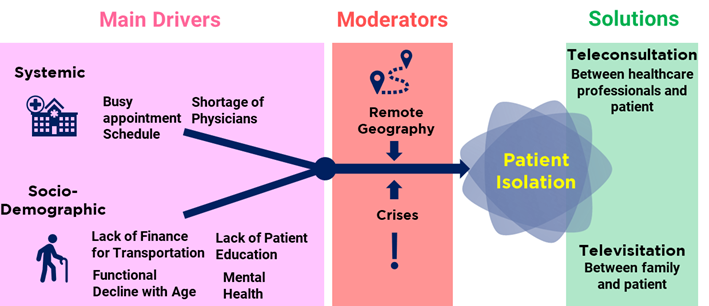
Anyone without access to care is considered an isolated patient, whether the reason for isolation is temporary or permanent. (This is not to be confused with medical isolation, where isolation is necessary to prevent the spread of disease.)

The obstacles that prevent people from accessing care can be categorized into four types: socio-demographic, geographic, systemic, and crisis-based. The first three types are permanent, while crisis-based obstacles are temporary.
Socio-Demographic Obstacles
- Limited understanding of care sites. Many people simply do not have the know-how to access healthcare. Either public awareness programs have failed them, or they don’t have the right support system to properly advise them on the actions they need to take.
- Lack of transportation to go to the healthcare facility. Having or arranging transportation, either private or public, is a major issue when it comes to accessing healthcare. There are people who do not have a car, do not have any public transport near them, and do not have the means to arrange transportation.
- Inability to reach out to mental health patients. Almost two-thirds of patients with a mental health diagnosis are not actually receiving treatment. There is still great stigma associated with getting help in these situations.
- Increasing immobility with age. This one is straightforward and compounds the isolation caused by the obstacles identified above. Many older people experience a decline in physical and cognitive functions. This makes it harder for them to move from place to place. Apart from the initial challenge of getting to a care site, there is the additional challenge of being alone when transitioned from one setting to another.
Geographic Obstacles
For many patients, geography is a significant barrier. In rural areas far from the nearest metropolitan centre, health problems are compounded by a lack of healthcare resources and limited access to transportation. A crisis can leave patients feeling far more isolated than in urban areas.
Systemic Obstacles
- Scarce appointment availability. Physician’s offices may not have hours that are convenient for all patients. Moreover, many physicians and staff have a heavy workload.
- Shortage of physicians. There is a general shortage of physicians right now, and this problem is expected to get worse in the coming decade.
Crisis-Based Obstacles
- Natural calamities. When there is a natural disaster like a hurricane or flood, some areas can lose health access coverage via loss of communication lines or transportation.
- Infectious spread. In the case of a virus outbreak like the COVID-19 pandemic, patients may be unable to access healthcare, not because they cannot make the trip but because medical isolation is preferred to contain the spread of the disease.
The Role of Telemedicine
Telemedicine is the virtual communications aspect of telehealth that helps to overcome the various obstacles to care, usually through video conferencing between patients and physicians. Its definition can be extended to communication between patients and other members of the care team as well, including caregivers and family members for added care coordination and emotional support, respectively.
Access to Healthcare Professionals
Teleconsultation allows people with financial or age-related limitations to access healthcare without having to set foot outside their door. This saves them transportation costs and is generally more convenient, especially if they have mobility issues. In times of crisis, even patients in urban centres can feel disconnected, but the role of telemedicine is magnified if the patient lives in a geographically isolated area.
Whether they live in rural or urban areas, if patients are not educated on care sites, a teleconsultation can be a great first point of contact to clarify where they should access care. In fact, it’s wise to include telehealth in any patient education strategy.
Teletherapy is used on a regular basis to reach mental health patients who might otherwise miss in-person appointments. In times of crisis, when their access to healthcare is temporarily severed, virtual communication technology allows these patients to continue their therapy sessions and stay connected to fight off loneliness.
Telemedicine also alleviates systemic limitations by helping healthcare professionals see patients more efficiently. Thus, a smaller number of physicians can tend to a larger number of patients, directly addressing the shortage of physicians. Virtual platforms also allow physicians to offer more flexible hours by removing the typical overhead costs of running a facility.
Access to Family and Friends
Finally, telemedicine helps to address isolation factors that go beyond access to healthcare professionals: connection with family and friends. After they are admitted to a facility, or when they are transferred from one setting to another, it’s important for patients to keep in touch with their loved ones. And it’s also a great psychological boost for family and friends to be kept in the loop on the patient’s care.
The word televisitation is used to describe instances when the family cannot physically be at the bedside of a patient in lockdown, and instead use virtual communications to interact with them. Televisitation can also be used to maintain contact with seniors in potentially lonely long-term care situations such as nursing homes and assisted living facilities.
Whatever the specifics of the situation, creating a regular communication schedule via virtual conferencing goes a long way to reducing the sense of social isolation and providing necessary psychological and emotional support.
Many thanks for reading. If you haven’t already, please consider subscribing to our blog by going to our blog page and scrolling down to the subscribe form. Feel free to share this post on your Social Media channels by using the share buttons at the bottom of this page.

