The virtual visit is the face of the telehealth revolution. Virtual visits, also popularly known as telemedicine, are video conferences between patients and physicians or other supports.
While other telehealth practices—such as the asynchronous exchange of information and remote monitoring—have seen different levels of adoption, virtual visits have caught on the most among the masses. In the United States, the adoption of virtual visits has risen over 50% in the last 5 years. They are expected to replace around 30 million in-person visits a year in the UK.
To ensure that telehealth projects run smoothly, it’s important for directors of virtual care to:
- Learn about the breadth of remote patient communication options
- Map outpatient journeys for various care scenarios
- Identify the various virtual visit touchpoints between the patient and the care team to set up an effective care pathway
Four Types of Virtual Visits
Virtual visits—using remote video communication—have become synonymous with telehealth thanks to the impact they’ve made on both healthcare organizations and healthcare consumers.
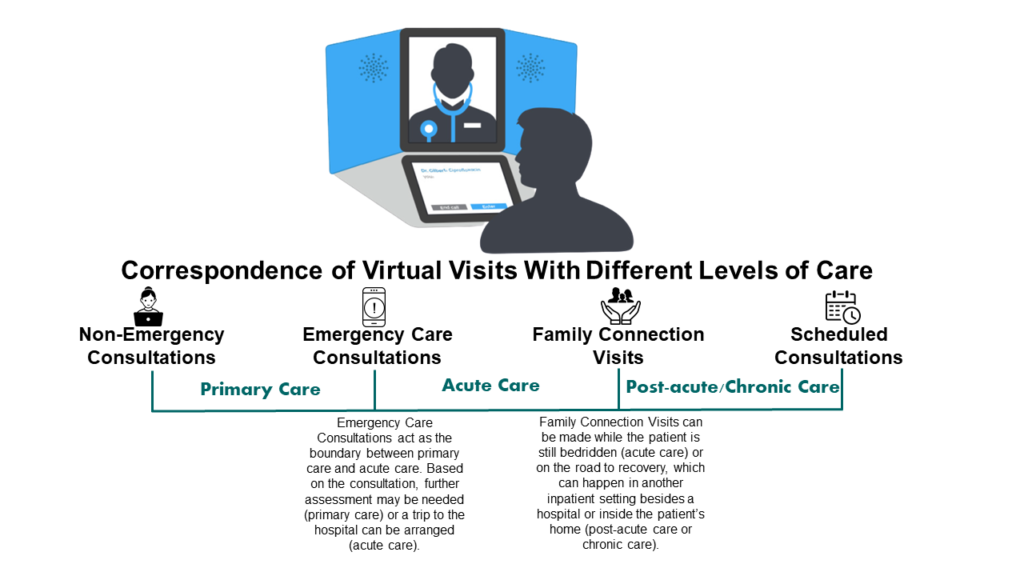
Not all virtual visits are the same. There are four types of visits, which touch all levels of care, spanning primary, urgent, intensive, and chronic care. These types are non-emergency care consultations, emergency care consultations, family connection visits, and scheduled consultations.

1. Non-Emergency Consultations
Kaiser Permanente is one of the largest healthcare insurers in the USA. Over half of Kaiser Permanente’s 100 million annual visits to the doctor are now conducted online over video. These include non-emergency urgent care, as well as routine primary care and specialist care.
Non-emergencies encompass a broad range of cases, ranging from the common cold to aches or swelling. Virtual visits with a primary physician or a specialist are currently offered under the same umbrella of virtual care services by all healthcare organizations that offer them.
Organizations do differentiate between first-time visits and established visits, and CMS has different codes in place for new patients and returning patients, respectively. It’s important to note that we are not counting e-visits and virtual check-ins as virtual visits, as both of these things can be done without live video, which is an essential component of a virtual visit.
2. Emergency Care Consultations
Nothing can replace dialling an emergency hotline number or visiting the emergency department (A&E in UK) in situations of immediate danger. But as a source of support at a critical moment, emergency care consultations come a close second.
These consultations are available 24/7, 365 days of the year, just like emergency rooms in hospitals. Nurses can triage patients over video to assess the appropriate level of care for them. Same-day access to physicians is possible if their expert opinion is required, and transport to the ER can be arranged.
Physicians can even consult with stroke patients by video inside ambulances, as every second counts when making an intervention in such cases. This practice has garnered enough popularity to merit its own term, Telestroke.
3. Family Connection Visits
This is the only type of virtual visit that is traditionally conducted in an in-patient setting, and between patients and families, rather than patients and physicians.
In an outpatient setting, patients and their family or social circle are able to maintain normal communication with each other, as they’re going home at the end of the day. But when they’re admitted overnight to a hospital, or permanently moving into a long-term care residence, patients’ communication with the outside world may take a backseat. Moreover, as they are in the custody of clinicians and care staff, communicating with families, caregivers, and the rest of their social circle cannot be left up to the patients anymore.
This is where virtual visits come into play. Tablets like the Samsung Galaxy and iPad are being used in intensive care units (ICUs) during COVID-19 to connect those under lockdown to their families. For example, we have collaborated with our partners in the UK on the Life Lines project. Thousands of video calls thus far have been conducted at over 150 hospitals to connect families to ICU patients.
4. Scheduled Consultations
Scheduled consultations are associated with a sustained episode of care. They usually take place long after emergency and non-emergency consultations, when the patient is on the road to recovery.
For example, patients recovering from surgery may need a number of virtual visit follow-ups to ensure the absence of complications and a return to normal life. Using the Aetonix aTouchAway system, nurses at Joseph Brant Hospital in Toronto are able to perform two checkup calls within 24 hours of discharge.
In other instances, a patient’s condition could be chronic and have to be managed with regular video visits scheduled over many months or years. Depending on the condition or the procedure, the need for such video consultations can be determined in advance and included as a part of the patient’s care pathway.
Many thanks for reading. If you haven’t already, please consider subscribing to our blog by going to our blog page and scrolling down to the subscribe form. Feel free to share this post on your Social Media channels by using the share buttons at the bottom of this page.

