How the Chronic Care Billing Codes Came to Be
Chronic care management in USA, ever since its inception in 2015 have created big waves in the treatment of those who are chronically ill. By incentivizing the treatment of those with two and more chronic diseases (and now one as well), Centers for Medicare & Medicaid Services (CMS) has offered physicians and hospitals to scale up this sort of care where there is a fee attached to the service. But it is not a traditional fee for service type of arrangement, which is tied to volume only. Rather it has a more value centric aspect to it, as this service is provided month in and month out, adding value to the patient’s quality of life. There have been many reimbursement codes instituted since 2015 which helps care providers understand what they can do for the patient, and what they can get paid for it.
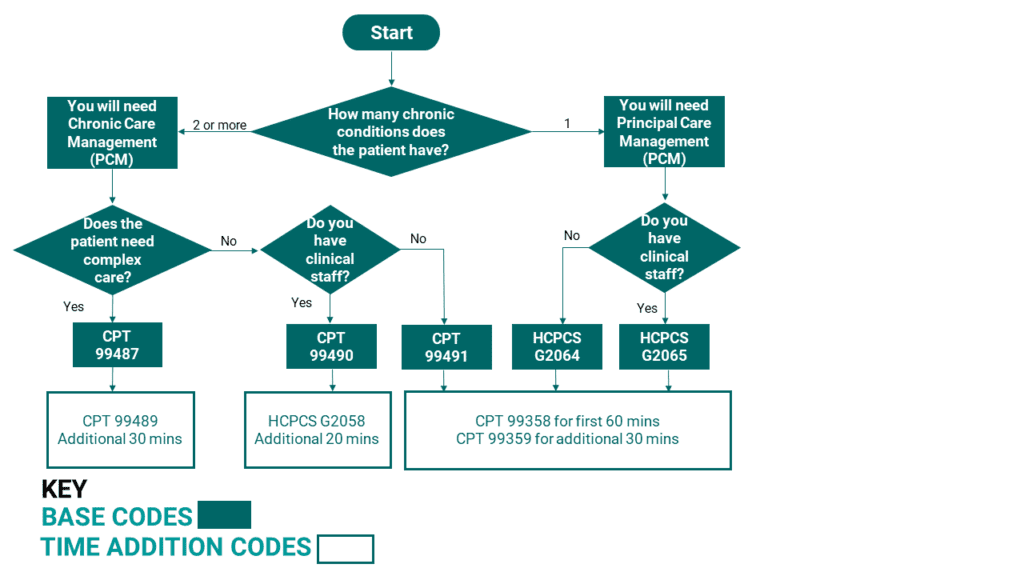
More important than the monetary aspect however, is how such reimbursement codes have given the American healthcare system a sense of structure on how to deal with patients suffering from chronic illness, as 45% if all Americans suffer from at least one chronic disease and it is responsible for three quarters of total healthcare expenditure. We have created an algorithm for these reimbursement codes to bring further structure to the treatment of chronic diseases.
Bringing Order to Chronic Care
While the chronic care reimbursement codes and other peripheral codes related to chronic care give the American healthcare system structure, it is not easy to recognize it as such if everything is displayed at once without any order to them. They are also updated every calendar year and some minor changes can at times have big implications in determining care options. If they can only be organized in a flowchart like fashion, it allows physicians and healthcare admins to get a feel for the type of programs that are possible. They can understand the options that are available to them to treat patients on an individual basis or group basis if a certain block of patients share the same situational characteristics. Thus, we have set out to do just that, creating a flowchart composed or rules that will lead one to the appropriate base code.
Base codes describe what must be done and for how long in order to bill using those codes.
Time Addition codes are billed on top of the base codes. They all have a time component to them as they are used when more time is needed in order to treat the patient.
Both base codes and additional codes are covered in chronic care algorithm diagram below.
Note: This Chronic Care Billing Algorithm is constructed from a patient’s point of view. The technical requirements of the codes are omitted such as who is eligible to bill and the actual reimbursement amounts. As are the definitions of the codes themselves. All such information is covered in our Chronic Care Reimbursement Guide posted on our reimbursement page. The purpose of this chronic care algorithm was to quickly decide on the care path of the patient. We thought it would be helpful to ask a series of questions that qualifies a patient for a certain type of reimbursement code, especially in light of all new changes that have been made recently.
The Three Potential Additions
The chronic care algorithm is already structured in such a way where you are advised on using one based code, and then additional codes for that base code if necessary. You cannot bill any two base codes together that are mentioned in the diagram. Which is why it is important to answer the questions to determine what is right for the scenario.
However, there are other codes in place which may be billed in the same month as those mentioned in the diagram. You will have to ask the following questions to see if the situation is applicable in the patient’s case.
Is the patient being transitioned at the same month? If so, you may be able to bill for it.
Transitional Care Management (TCM) Codes exist in order to bill for transitional care services. CPT 99495 can be used if there is at least moderate complexity decision making at play. CPT 99496 is used if there is high complexity decision making at play and the first face to face visit is scheduled within 14 days. There is a way to bill for transitional care management and chronic care management (CCM) in the same month. If the 30-day post discharge service period for TCM ends before the calendar month, and the CCM requirements are met from that time onward to the end of the month, you will be able to bill for both.
Will the patient need to be remotely monitored for 16 or more days a month as well?
There were three remote patient monitoring codes instituted in 2017 which can be billed in the same month as chronic care. It’s only a matter of understanding if the patient’s case requires the remote monitoring of vital signals. The three codes are CPT 99453, which is for setting up and educating the patient, CPT 99454 which is for the actual monitoring of the patient, and CPT 99457 which is for the management services on part of the physician or staff. Recently, CPT 99458 was enacted as time extension code for remote patient monitoring services.
During the initiating visit, is there sufficient time spent on Care Plan Development?
An initiating visit will be required to embark on any of the paths mentioned on the diagram. It’s important to note that those visits can also be separately billed. But on top of that, if additional work is required in developing a care plan when initiating a patient, you will be able to bill for HCPCS G0506. It’s a one-time fee.
Many thanks for reading. If you found the content useful, please consider subscribing by navigating back to the blog page and scrolling down.
