
Patient Care Coordination is the deliberate organization of people, activities, and processes to make healthcare more effective, efficient and safe for patients. More effective healthcare results in more positive health outcomes. More efficient healthcare results in greater patient and clinician experiences. It also applies to being cost-effective where you are budgeting public funds to manage the health of a population. Lastly, safety is paramount, and it is important to ensure the safety of both patients and clinicians when providing and receiving care respectively.
Where does the need for care coordination stem from in the first place? It’s because in any healthcare system, there are multiple organizations and multiple occupations, all of whom are entrusted to coordinate care for the patient. But if one is to achieve the triple aim for better outcome, lower cost, and better experience, there is no other way to achieve this without a proper care coordination system in place.
Evolution of Care Coordination
Care coordination has always existed, but ever since the rapid advent of telecommunications in the late 20th century, it has become a science of its own called Connected Health, as the technology is readily available to connect different healthcare stakeholders who may not be in the same location. The three biggest stakeholders in care plan are the patients, the healthcare professionals and the caregivers, which can include family and friends. In order to facilitate information exchange among them, technology such as handheld devices, apps and the internet have become ubiquitous in their application. Telehealth has caught the healthcare world by storm, which is simply Connected Health at a provider to patient level. By adding more members to the patient-physician dyad, one can enlarge their care coordination network and take it to the next level.
Virtual Care Coordination

This article will focus on the telehealth aspect of Care Coordination, which we are calling Virtual Care Coordination. It includes telemedicine (video conferencing, texting and store and forward technology), remote patient monitoring (measuring vital signs) and mHealth (the use of mobile phones or other hand held devices in Connected Health). In order to truly live up to the aims of care coordination, going virtual is a necessary mandate. There is also an argument to be made from the patient’s perspective for virtual care coordination, which is despite knowing right from wrong, people are prone to self-indulgence and habit formation. So having a third party control by means of virtual technology that gives constant feedback and support motivate people to adhere to their care plan and change their lifestyles.
There are 4 main components of virtual care coordination. Engagement, that consists of pleasant interactions that encourages acceptance and long-term usage. Education, that consists of relevant and timely information for patients that allow them to follow the prescribed care plan and implement lifestyle changes. Evaluation, which consists of clinicians remotely assessing improvements, detecting setbacks, and intervening as necessary. Empowerment, which consists of enabling patients to manage themselves and live as independently as possible.
Virtual Care Coordination Adoption
The percentage of hospitals with full or partial telehealth systems have doubled in the last decade, with 76% of all hospitals having implemented video conferencing capabilities to mete out care. But having the technology is only one half of the battle, it is the providers and patients who have to use them. 23% of physicians say that patients are not interested or don’t have the technology to support virtual care, and 35 % of them say that their workplace does not offer the required technologies. Even in organizations that have implemented the technology, 33% of them say that they don’t expect usage to increase for physician-to-physician electronic consultations, 27% of them say the same for email/patient portal consultations, and 20% for data from patient wearables. Thus we see that while telehealth has arrived, it is still being used reservedly which is hampering virtual care coordination. When one better understands all the different places and actors involved in the healthcare landscape, they will see that they have no choice but to use technology or virtual case, for the sake of optimizing patient care coordination. We hope to do that in post in three steps.
The 3 Steps: Levels of Care, Best Practices and Current Models
We first discuss the levels of care that are usually found in all the health systems of the world. The types of locations involved at each level will be mentioned, so we have an idea of how the patient journey is like traversing through these levels of care. After all, as stated before, care coordination only exists as there are multiple organizations and multiple occupations.
After we have mastered our understanding of the levels of care that are available, we cover the essential things that you have to do in all levels in order to truly check all the boxes for virtual care coordination. You may see these as best practices.
Lastly, we explore three models of care coordination that are out there that have been made possible by the use of technology. One can implement these models when building the care coordination program that befits their healthcare organization. Keeping all the levels of care and considerations of each level in mind from steps 1 and 2, it is possible to further improve on these models of care coordination.
Step 1: Understand the 4 Levels of Care
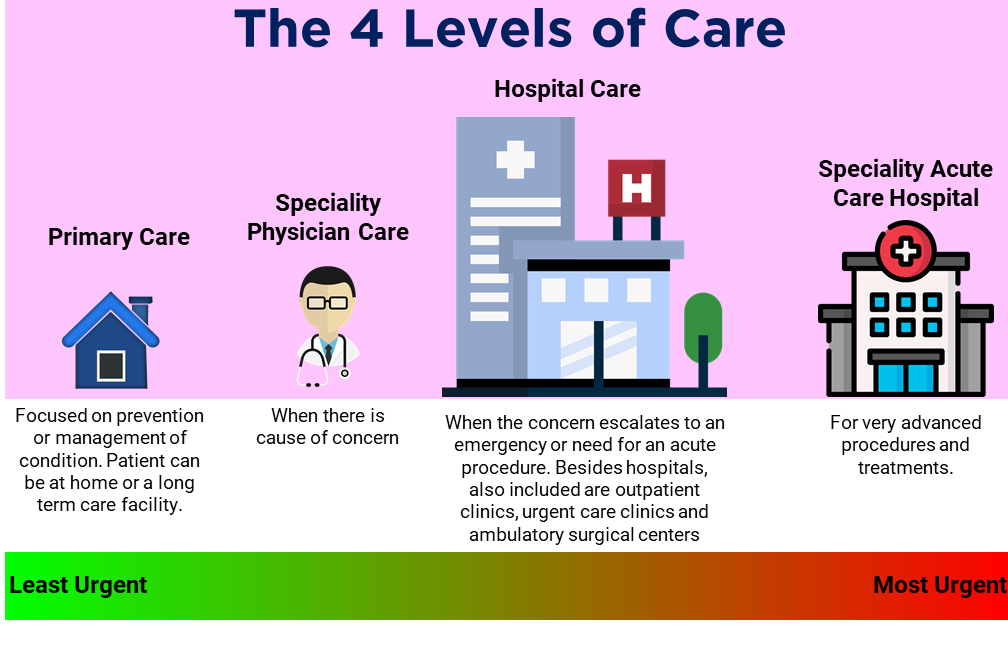
A NEJM Catalyst report on care coordination had found that only 7% of healthcare organizations claim to be fully coordinated between inpatient settings, post-acute setting and at-home setting. More than half of healthcare organizations claim to be somewhat coordinated, and 10% of healthcare organizations claim not to be coordinated at all. We shall discover what all these terms mean in the following paragraph.
1st Level
Primary Care is the first level of care. It is administered by a family or personal physician, usually inside an office. It provides comprehensive healthcare for people of all ages. It is also referred to as general practice. Primary Care physicians, Family physicians or general practitioners can manage the health of a person or family by addressing concerns and recommending preventative measures to maintain general wellness. Annual wellness checkup programs are often a part of the care in this level. One could receive primary care all their lives, without ever having an emergency or a serious diagnosis. Coordination is relatively simple at this stage, as you are only dealing with your primary care physician’s office.
Location: Physician’s Office. Can be at a private practice or an outpatient clinic. Can also be conducted from the patient’s residence.
2nd Level
Specialty Physician Care is the second level of care. The family physician or general practitioner will consult with specialists if it’s an area of treatment beyond their scope of expertise. They may also refer the patient to such a specialist in a medical field where a diagnosis or treatment is required. Such care is still received inside of offices, either private practices or inside healthcare facilities. It helps to be close to diagnostic facilities which will have the necessary equipment to do X Ray, blood tests, urine tests, cranial scans etc. There is likely cause for precaution or concern at this stage, as it requires the expert opinion of another person who will now be privy to your care. Any emergent issue, gradual or sudden, that has to be dealt with may require the collaboration between two or more physicians. Short of being an acute emergency, which has to be dealt with immediately, all other symptoms would still go through primary care first.
Location: Physician’s Office. Can be at a private practice or an outpatient clinic.
3rd Level
Hospital Care is the third level of care. The goal in life is perhaps to be healthy and lucky enough where a person never has to end up in a hospital. But things happen, and one may be referred by the primary care physician or specialist to an outpatient or inpatient hospital service. If 24 hours of care is required, that is, overnight hospitalization, the patient is referred to an inpatient facility or more commonly known as a hospital. In such a facility, the patient gets a hospital bed. On the other hand, if they do not need continual supervision, you are referred to an outpatient clinic or ambulatory surgery center. Some outpatient clinics may be in the first floor of a hospital or at a separate facility. The difference between inpatient and outpatient is thus not so much the location of care, but rather the duration of care that the patient receives.
One may directly access emergency care in hospitals or urgent clinics if they need help immediately and are unable to go through their primary care team. Emergency Rooms or Emergency Departments in hospitals will have equipment such as a CR or MRI machine, and will always have physicians on staff. They operate 24 hours. An urgent care clinic may only have access to an X ray machine if that, and some are only manned by physician assistants and nurse practitioners. They are for non-life-threatening injuries like infections, allergic reactions, fractures and lacerations. An ambulance crew can do some of the things that an urgent care clinic can, and so one should always aim for the ED to save lives. Especially if it’s a case of anaphylactic shock or serious breathing problems. Going to the urgent care center with life threatening cases will result in them putting an IV on you and sending you elsewhere.
Location: Hospitals. Outpatient Clinics inside or outside hospitals. Urgent Care Clinics. Ambulatory Surgical Centers.
4th Level
Specialty Acute Care Hospital is the fourth level of care. As opposed to the third level, this level is comprised of exclusively in-patient care as specialized physicians and equipment are needed to restore the patient’s health. Examples of procedures include coronary artery bypass, renal dialysis, neurosurgeries and cancer treatment.
Location: Medical Centers.
Step 2: Things That you Have to do at All 4 Levels of Care

It is important to keep in the mind that the levels of care in step 1 are all based on the person’s need. In all four levels, the patient’s starting and ending place is their home. Either they get the care they need and return home the say, or they return home after their stays in hospitals or medical centers for more serious cases. Home in this case does not only mean private houses and apartments, but also retirement centres, nursing homes and hospices. The four levels of care can be coordinated from the patient’s place of residence, whatever that place is. But despite where the patient lives, it is important to do the following things when accessing and moving between the levels of care.
Establish Accountability and Responsibility
This will be dictated by the health system that treats the patient. The payor may be the private insurance companies or the government, but that is another subject that is beyond the scope of this guide. The bottom-line is that whoever the payor is, they would want an efficient system where the patient can quickly access the level of care that they need, and that they can be subsequently managed for health restoration or mitigate further deterioration, whatever the situation mandates. Everyone involved in the system must know their role and assume the responsibilities that come with it.
Important Considerations
The patient has a responsibility to see care if they are not feeling well. They have to make an appointment with their primary care physicians. If the hours of operation is an issue, they can try walking into a retail clinic. Urgent care clinics have friendlier hours than private practices. The patient also has the responsibility of adhering to whatever care plan that is prescribed.
The caregiver has a responsibility to assist the patient as needed. This person could be anyone, but ideally a family member or friend. Home health aides are also available commercially. They could provide physical, morale and informational support to ensure that the patient gets the care that they need.
The care coordinator, if such a person comes into contact with the patient, has the responsibility of educating both the patient and their caregiver of all the services and products that is available to them. For patients with complicated histories, the care coordinator would know how to dispense the best resource possible, whether that be specialized skills, medication or access to equipment.
Communicating/Sharing Knowledge.
The patient and the caregiver must have a way to keep in touch with a designated point of contact. Telephonic communication does not cut it any longer because you lose the ability to communicate asynchronously where both parties are not together in real time. By incorporating store and forward technology and instant messaging, you ensure that whenever each party has an update, they can communicate it to the other side instantaneously without worrying about forgetting it later. If it’s an emergency, then they call their designated contact. Video calling is better than telephonic communication as you are able to see the patient as well. mHealth devices such as smartphones and tablets are best for this, from where you can make video calls but also have a platform for sending and receiving information asynchronously.
Important Considerations
Communication is absolutely crucial. If Care coordination is a property, communication is the unit of measurement to measure this property. So the importance of having proper infrastructure in place cannot be stressed enough. Every person involved in the care team must have a device through which they can send and receive information. For physicians and care coordinators, this can be their work computers or smart phones. They would have access to an EHR system and a patient portal. From the patient’s and caregiver’s perspective, they can either use their own device and download an app of sorts, or they could receive a device preconfigured with the patient platform technology that is being used. But they must have such a device at the bare minimum.
Figuring out the accessibility of devices is a crucial component of virtual care coordination. The 50- to 64-year-old demographic is often the age when chronic conditions begin. Starting this segment on a preventive and proactive CCM program early on using mobile technology is a step toward preventing issues in the future. They still may be technologically savvy at this age to use mobile phones to participate in their care plans. For the folks that are older, larger screen such as a tablet or even their home PC screen may be more appropriate. If anyone is incapable of using a device, then that responsibility is shifted to their caretakers who many need to be upskilled.
Creating a Care Plan that Includes Assessing and Supporting Patient Needs and Goals
A Care plan is necessary at every level of care! If communication is the measuring unit of care coordination, then a care plan is the fuel which sustains it. An assessment of patient needs, forming goals around that need, and routinely following up and responding to changes of patient’s needs are all things that begin with forming a care plan. Even for the most benign of cases, it helps to keep that record as a part of the patient’s EHR, so it can provide context for future incidences. As far as wellness and prevention services go, it is a no brainer to develop and maintain a care plan for a person in the hopes that no complications occur because of lifestyle choices, and that they never have to be referred to higher levels of care.
Since it is understood that the first level of accountability lies with the patients themselves to maintain a certain lifestyle or adhere to the care plan, they must be supported with resources so they can be pro-active in maintaining their health. Alternatively, if they are coming off a major surgery or hospitalization in ER, they similarly need to be supported with resources in order to rehabilitate them into their normal lives or adjust to their new permanently altered conditions.
They can be linked with community resources that facilitate their care plans. They include:
Meal Delivery Services
Whether it is to improve diet, or because they are unable to cook, meal delivery services give recovering patients a source of nutritional food that is delivered to their door, saving them the logistics headache.
Community Exercise Programs
Being active is a staple recommendation for most care plans where the patient is able to move. Gyms and fitness centers can be made available for workouts. Classes in friendly settings for similar patient bodies can be arranged where mobility and balance are improved.
Counselling Programs
Depression is listed as a chronic disorder for a reason. It often accompanies some of the order chronic disorders related to the heart and lungs. Opioid abuse is a growing problem around the world. Both depression and addictions are not just related to the physical health, but mental health as well. It is very important to have access to services that deal with grief, loss, psychological distress and regular challenges that accompany recovering from a procedure or living with a chronic or debilitating condition. Medication Assisted treatment comprises of medication and behavioral therapy to treat substance abuse disorder.
Rehabilitation Programs
This is closely related to Community Exercise Programs, but is more clinical in nature. In many post-acute care settings, going to a rehabilitation center is not optional but a part of the care plan. Occupational and physical therapists are trained to help patients recover from trauma and restore their cognitive and motor functions.
Community Immigrant Services
Sometimes in the proper comprehension and execution of a care plan, culture or the language barrier becomes a major issue. Luckily there are programs in place offered by community Immigrant services which attempt to quickly get the patient up to speed on the areas’ language and customs. Note that a a truly personalized care plan would have already accounted for the unique life circumstances of the patient. But it always helps to learn more about one’s surroundings to gain confidence.
Adult Day Care
Adult Day Care centers provide supervision for senior citizens. It provides the mental and social stimulation outside of their households, and give their caregivers a much needed break. The staff on site can help with grooming, walking, feeding etc.
Remote Patient Monitoring Programs
If patients’ vital signs such as temperature, pulse rate, respiratory rate, oxygen saturation level, blood glucose and blood pressure are to be monitored remotely, they will need to be coached on the use of the new devices and platform to read and transmit the information. It is important to ensure that readings are logged into EHR, and alerts are sent to clinicians when they fall out of normal range. The data points described above are most commonly measures in RPM, but other data can be measured too such as sleep patterns and body positions for patients with sleeping disorders, and mobility for patients with arthritis.
All of the above programs consist of more healthcare professionals, social workers or even just regular civilians being added to one’s care team. Thus, it is imperative to establish shared expectations between providers and the many community agencies.
Have a Contingency Plan for Sudden Escalations
If a patient requires emergency care, there should be a transition plan in place by which the patient can be taken to the nearest emergency department of a hospital. Such a plan can include contacting emergency contacts who could give them a ride, or arranging an ambulance with paramedics to receive pre-hospital emergency care. If it requires the consultation of a specialist at this time, video calls can be arranged with specialists inside of the ambulance. We see this in treating stroke patients in what is called teleneurology, where immediate lifesaving decisions are made on the fly via video consultations.
Important Considerations
There is setting, and then there is the level of care. A patient can be at any setting, and experience going through all the levels of care at the drop of a time. So there should be proper connectivity via electronic information exchange pathways between all these facilities. These include physician’s offices, hospitals, clinics, medical centers, homes, long term care agencies, rehabilitation and even all the community agencies. A patient could be temporarily or permanently be placed in one of these settings, and require access to other settings in a hurried manner. Hence, such facilities must be ready to transition the patient to a higher level of care if they are incapable of handling the emergency at hand.
There is no on and off switch for caregivers in virtual care coordination. Normally, caregivers may need to coordinate care only when their family member is discharged after receiving acute or emergency care, or when there is a communication breakdown, or when extra help is required. In a virtual care program, you have to have the mental set up to be ready to help whenever you are called upon.
Step 3: Agree on a Model

Models of Virtual Care Coordination
There are three main models of care coordination. All of them rely on virtual connections for their day to day and long-term administration. They are:
1) The Guided Care Model.
2) The Integrated Care Model
3) The Patient Centered Medical Home
The purpose of step 1 and step 2 was to understand all the different agencies and components that goes into the care coordination of the patient. Hence you are not limited to the three models as mentioned above. When designing your virtual care coordination model, you may borrow ideas from all three, but come up with your own unique virtual care coordination model that suits the relevant needs of your organization and patient population. These three models are there to guide you and give you a template to start building your care program or modify it to your particular context.
1) Guided Care Model: A Guided Care Model is designed for primary care practices. It helps them meet the complex needs of patients suffering from multiple chronic conditions. In a guided care model, the RN quarterbacks care coordination for the patient. They perform initial assessment of the patient, collaborates with primary care providers to develop a care plan and makes sure that the patient adheres to the plan, connecting them to specialty care providers if required. The RN is entrusted to guide the patient through their care journey, escalating a case for an on-site visit if required.
While primary care can be relied upon to handle chronic care management, what happens if the patient is need of acute care which is critical in nature? If not that, then at least an episode of care that requires immediate attention that goes beyond a gradual deteriorating of symptoms that can be managed?
When a patient suffers from such sudden situation, such as a stroke or heart attack or early symptoms of the aforementioned, there is a risk of coordination break down as they may first receive care from a location that is outside of their regular care network. Thus communication between providers during hand offs in pre admission and the transition of care post discharge is crucial. In instances of post-acute care, where the patient is not discharged directly to their homes, they may first be placed in long-term care facility, or rehabilitation facility of which there are many types. Collectively these facilities are known as post-acute care facilities. Hospital discharges to post-acute care facilities have increased in recent times. Many patients are transferred from one post-acute care facility to another before returning home. In some cases, these post-acute facilities are their new permanent homes. So there is a great degree of coordination required between these institutions so the patient transition is seamless.
Takeaway: The nurse is the perfect person to coordinate care in a Guided Care Model due to the mixture of hands on but also operational expertise. As they are usually operate in primary care, the are already familiar with the patient, so in the event something goes wrong, they can best coordinate secondary care for them. Then when they have recovered, and it’s time to settle back into normal life, the familiarity of patient-nurse relationship comes into effect once more. They can either resume primary care if it’s something like recuperating from a scheduled surgery. The nurse will check progress via virtual visits, schedule follow up visits if necessary and help to order new medications for change in any prescriptions. If it’s a more life-threatening condition where the patient’s health is permanently altered, then they will require tertiary care where the chronic disease now has to be managed for stabilization. In such a case, there is need for greater coordination. Luckily for the nurse, them knowing the patient will help them suggest the right support facilities for them, in which they are more likely to partake in. These include nursing homes and rehabilitation centers.
2) The Integrated Care Model: Integrated care is a multi-disciplinary team-based model of care that includes the patient’s family as well in the care circle. The healthcare professionals rely on each other’s expertise and the input of the family members to develop a personalized care plan for the patient.
Perhaps, more than any other care scenarios, patients suffering from severe mental health issues like Alzheimer’s or dementia need the highest level of care coordination, because not only can things turn left very soon as with high risk chronic patients, but these patients are cognitively unable to take the right decision if push comes to shove. In a peer reviewed study which analyzed all care models for such scenarios and found that they all had some common elements. They relied on a care coordinator who can either be a RN or social worker. The multidisciplinary care team includes the primary care physicians, specialists, therapists, pharmacists, and psychiatrists. They all involved a structured needs assessment, a care plan to be followed, care coordinators referring or directly arranging care for the patient, and ongoing monitoring and support, which involves counselling, support groups or other therapy.
Takeaway: The Care coordinator, also called navigators take the lead in the Integrated Care Model. They work one on one with the patient to help them access the care they need, and when they need it, as stated before. It is important for the virtual platform to be set up with as many stakeholders as possible available at the fingertips. This makes the job of the care coordinator much easier, which is crucial as they are entrusted for not just quarterbacking the care for the patient as with the Guided Care Model, but effectively controlling the strings of the whole care operation. Sometimes confused for a case manager, a care coordinator applies more to the entire patient journey, where as a case manager role applies to more a single episode of care in one facility.
3) The Patient Centered Medical Home : The Patient Centered Medical Home model provides relationship-based comprehensive care to the patient that includes primary care, acute care and chronic care. Partnering with the patient and their family involves understanding their unique needs, culture and preferences. The patients and family members are treated as the core members of the care team, and so they are kept fully informed of care plans. The PCMH model emphasizes open communication among the patient, their families, and other facilities in the larger health system which may have interactions with them or treat them. Accessibility is a huge part of PCMH model, where the objective is to reduce waiting time for urgent needs and around the clock telephone, video call and email support. Ongoing quality improvement through evidence-based medicine and clinical decision-support tools are used to guide shared decision making. The primary care physicians are in charge of the patient-centered medical home, and are aware of the status of all referrals and transitions of the patient.
Takeaway: The primary care team takes the lead on The Patient Centered Medical Home (PCMH), but unlike The Guided Care Model, where a lot of the responsibility is heaped on the RN to be the coordinator, it is usually the primary care physicians that coordinate care. Overlaps between the models of care coordination are bound to happen, and the terms are even used interchangeably at times, but generally PCMH is the most comprehensive model out there that takes into accounts more specialties than any other other. Instead of just being just multidisciplinary like The Integrated Care Model, it is interdisciplinary which means that the various specialties do not just work together for the sake of the patient, but there is a synthesis of their knowledge. The PCMH will look to partner with professionals and teams in other settings to devise a care plan for the patient. Anyone who participates in the patient’s care plan including at times of care transitions will be included in this group.
Conclusion
Physicians know how to do their jobs. There are tips for care coordination listed for physicians such as considering other conditions when prescribing medications, and for patients such as bringing a list of medications to appointments. But such minute best practices should already be covered in education from the get-go. The role of care coordination is to not really teach people how to give and receive care. It is to set up a system in place, whereby you can practice efficiently knowing all your ground rules will be adhered to a mass level to handle all situations. By implementing the three models discussed in the article, you can achieve patient-centered care coordination that takes into account multiple levels of care, and different actors and facilities. If you are looking for more specific models, check out this page on the Rural Health Information Hub.
As the scope of virtual care coordination is so broad, it may be wise to adopt an enterprise approach in selecting an area of concern that is to be addressed. First, determine what your most pressing needs are. Then organize and consolidate your resources to coordinate the type of care that will help you with that concern. Examples include chronic disease burden, transition between facilities and levels of care, referrals and healthcare professionals shortage.
When adopting virtual care or telehealth to enhance care coordination, you will need a centralized team that provides the core services such as technology rollout and support. Make sure you go over how your care coordination challenges around the identified problem areas will be met by the new technology. For chronic care burden, ask how the technology will help who are at high risk vs those who are projected to be at high risk in the future, and are labeled rising risk currently. It has been found that focusing on rising risk patients will reduce their conversion to high risk by 6 percentage points, and result in a positive 3-4% margin in 5 years. For care transitions, ask what level of involvement can be expected from the primary care team which was found to be instrumental in solving real-time communication, which is cited to be to the biggest challenge for care settings. For addressing healthcare professional shortage, ask how much of the 70% of care coordination that is done face to face will be shifted to virtual care.
It’s our belief that by understanding the levels of care, identifying the organizations and people the patient will come into contact with, establishing a list of activities at each of those levels, and by tying it all together via an evidence based model, you will be well on your way to achieving virtual care coordination.

